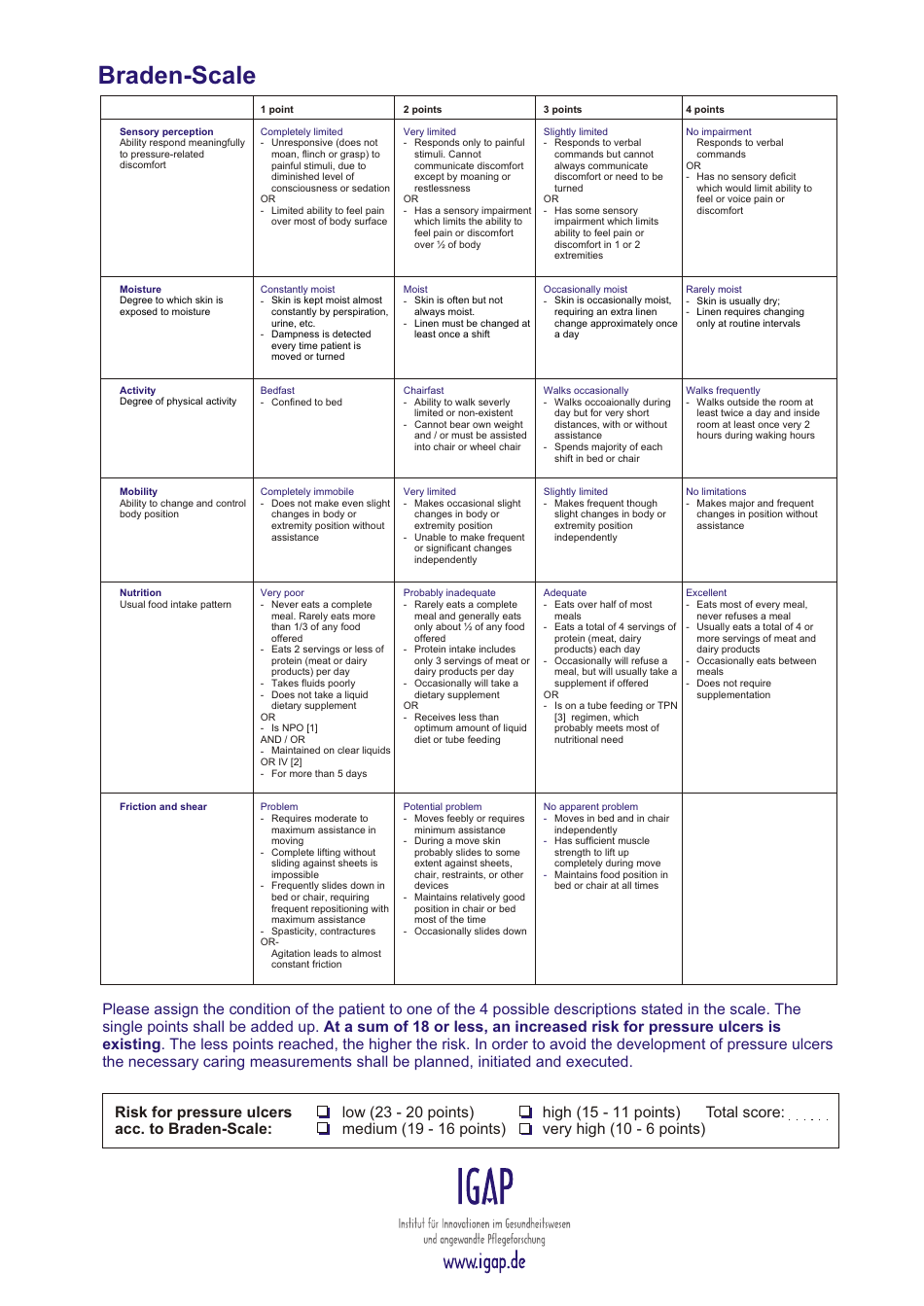
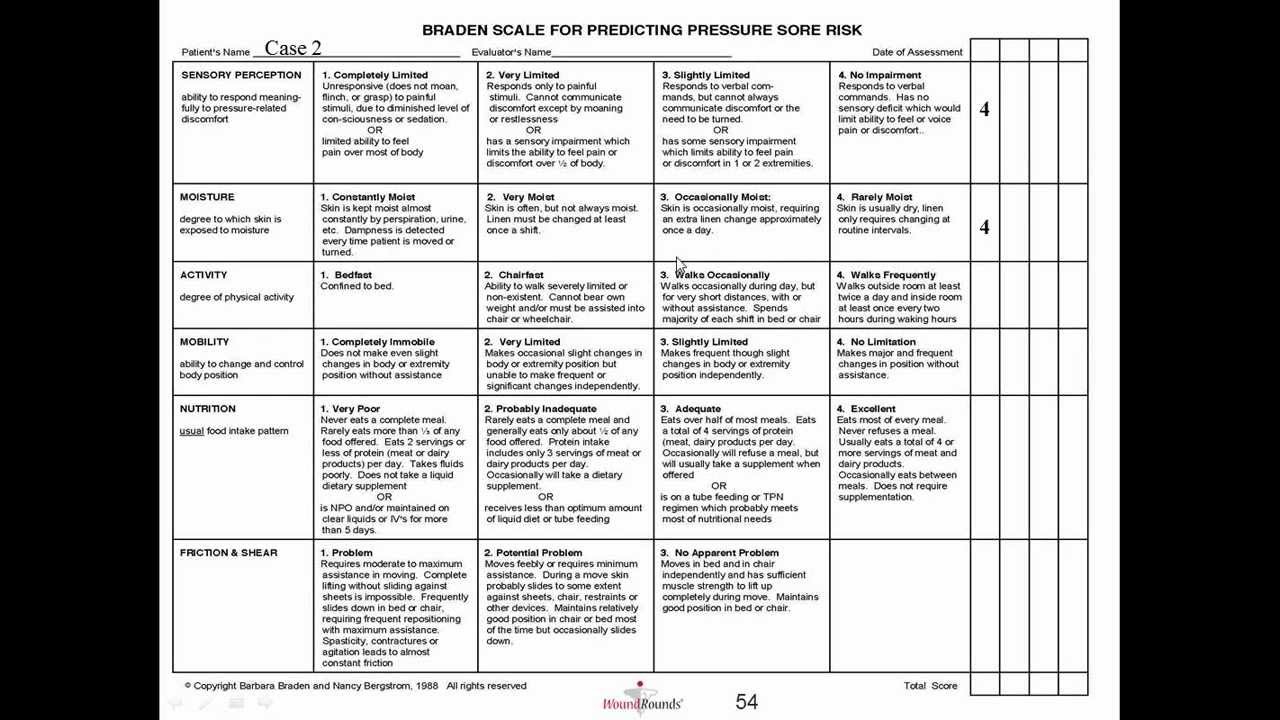
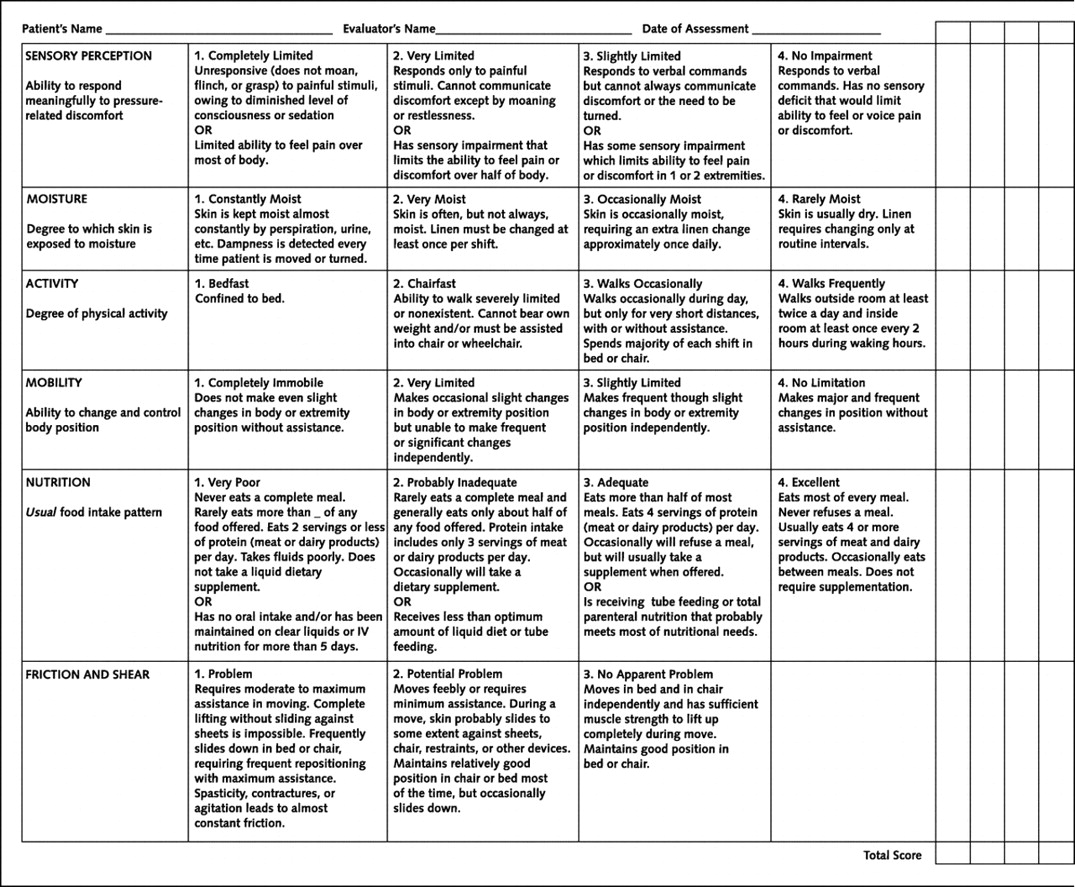
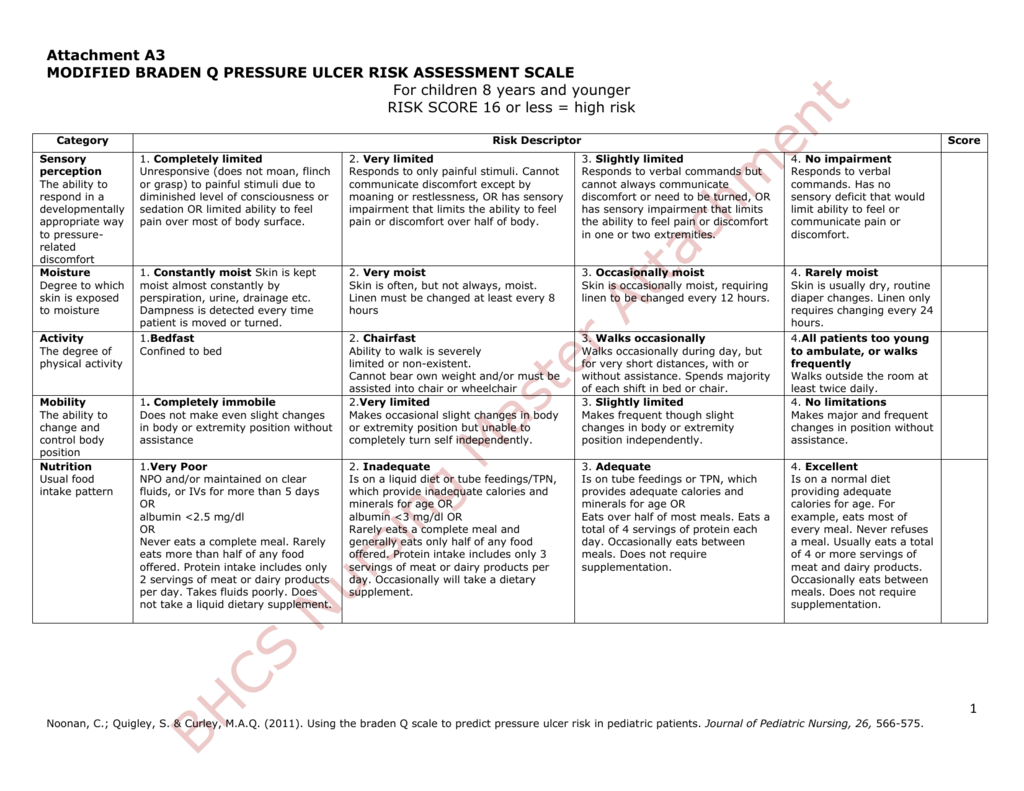
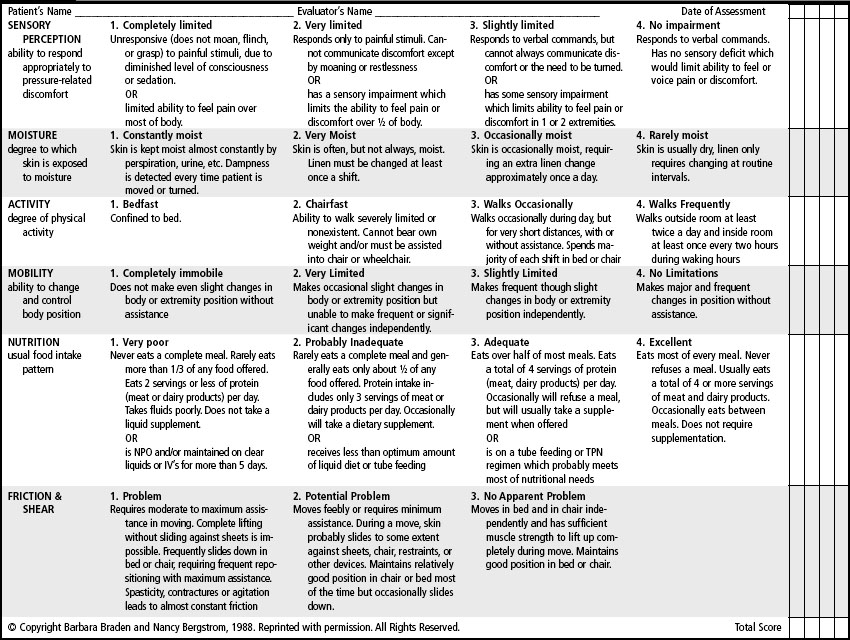
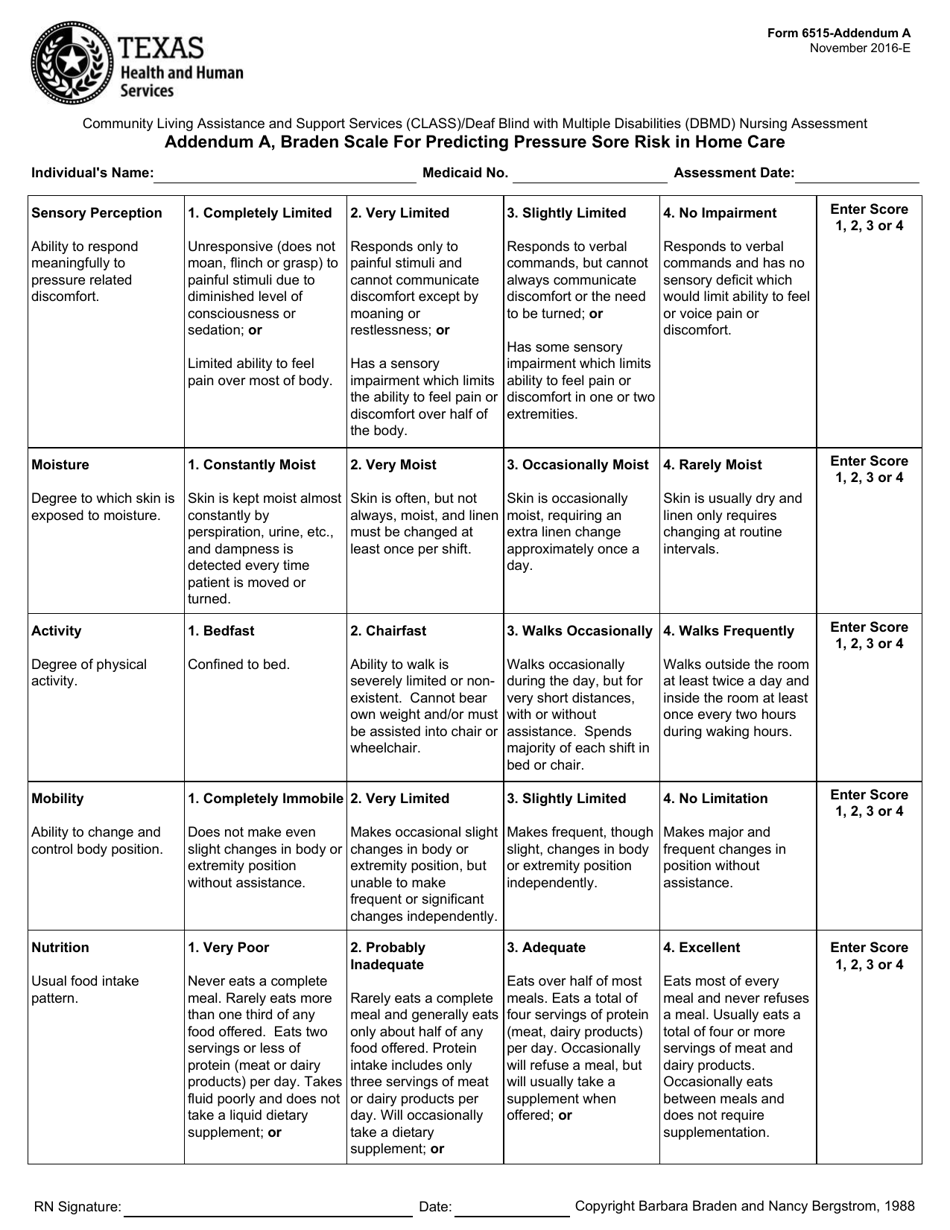
Protocol for braden moisture subscale developed by dr. The braden scale for predicting pressure sore risk background: Braden scale for predicting pressure ulcer risk category i (stage i) category ii (stage ii) category iii (stage iii) category iv (stage iv) unclassified (unstageable) suspected deep tissue injury. Barbara braden and nancy bergstrom. Braden scale for predicting pressure sore risk.
Dampness is detected every time patient is moved or turned. Braden scale for predicting pressure ulcer risk category i (stage i) category ii (stage ii) category iii (stage iii) category iv (stage iv) unclassified (unstageable) suspected deep tissue injury. Sensory perception, moisture, activity, mobility, nutrition, and friction or shear. If any of the six subscales have a score of 1, 2 or 3, it may indicate a higher risk for skin breakdown. The braden scale (developed by braden and bergstrom in 1987) stratifies risk of the patient developing pressure ulcers or injuries based on six categories or subscales:
The braden scale has proven to be highly effective in assessing the risks for hospital acquired pressure ulcers (hapu) among patients in medical, surgical, and critical care settings. Protocol for braden moisture subscale developed by dr. Empower caregivers to look beyond the total braden scale score—and look more closely at the subscores. Skin is kept moist almost constantly by perspiration, urine, etc. The evaluation is based on six indicators:
See figure 10.21 [1] for an image of a braden scale. Braden scale for predicting pressure sore risk. The braden scale for predicting pressure sore risk background: The braden scale is a scale that measures the risk of developing pressure ulcers. Dampness is detected every time patient is moved or turned. Unresponsive (does not moan, flinch, or grasp) to painful stimuli, due to diminished level of consciousness or sedation. Or limited ability to feel pain over most of body. Risk assessment is a central component of clinical practice aimed at identifying individuals susceptible to pressure injuries in order to target appropriate interventions and prevent pressure ulcer development. Risk factors are rated on a scale from 1 to 4, with 1 being “completely limited” and 4 being “no impairment.”. The braden scale for predicting pressure sore risk should be conducted for the purpose of planning preventive interventions and that the prevention plan should be based on assessment of individual braden subscale scores. The braden scale (developed by braden and bergstrom in 1987) stratifies risk of the patient developing pressure ulcers or injuries based on six categories or subscales: Individuals with a score of 18 or less are considered to be at risk of developing pressure ulcers. Skin is kept moist almost constantly by perspiration, urine, etc. Braden scale for predicting pressure sore risk. Proceed by completing applicable information for each numbered site on chart to include ostomies.
Responds Only To Painful Stimuli.
Use the braden scale to assess the patient’s level of risk for development of pressure ulcers. Barbara braden and nancy bergstrom. The braden scale, developed for formal assessment in the late 1980′s, rapidly became the most commonly used tool for assessing pri risk in most united states healthcare settings. The braden scale for predicting pressure ulcer risk, is a tool that was developed in 1987 by barbara braden and nancy bergstrom.
It Has Proven To Be More Accurate Than Relying Only On The Clinical Judgment Of Nurses.
Proceed by completing applicable information for each numbered site on chart to include ostomies. The braden scale for predicting pressure sore risk should be conducted for the purpose of planning preventive interventions and that the prevention plan should be based on assessment of individual braden subscale scores. Permission should be sought to use this tool at www.bradenscale.com. The braden scale is a scale that measures the risk of developing pressure ulcers.
Unresponsive (Does Not Moan, Flinch, Or Grasp) To Painful Stimuli, Due To Diminished Level Of Consciousness Or Sedation.
If any of the six subscales have a score of 1, 2 or 3, it may indicate a higher risk for skin breakdown. Sensory perception, moisture, activity, mobility, nutrition, and friction or shear. Individuals with a score of 18 or less are considered to be at risk of developing pressure ulcers. The scale consists of six subscales that reflect determinants of pressure (sensory perception, activity and mobility) and factors influencing tissue tolerance (moisture, nutrition and friction and shear).
The Braden Scale Has Proven To Be Highly Effective In Assessing The Risks For Hospital Acquired Pressure Ulcers (Hapu) Among Patients In Medical, Surgical, And Critical Care Settings.
Braden scale for predicting pressure ulcer risk category i (stage i) category ii (stage ii) category iii (stage iii) category iv (stage iv) unclassified (unstageable) suspected deep tissue injury. Braden scale for predicting pressure sore risk. The evaluation is based on six indicators: Protocol for braden moisture subscale developed by dr.